When it comes to UX design, healthcare has to be one of the areas where it’s most critical that it’s done right. The difference between good and bad design could literally make the difference between life or death.
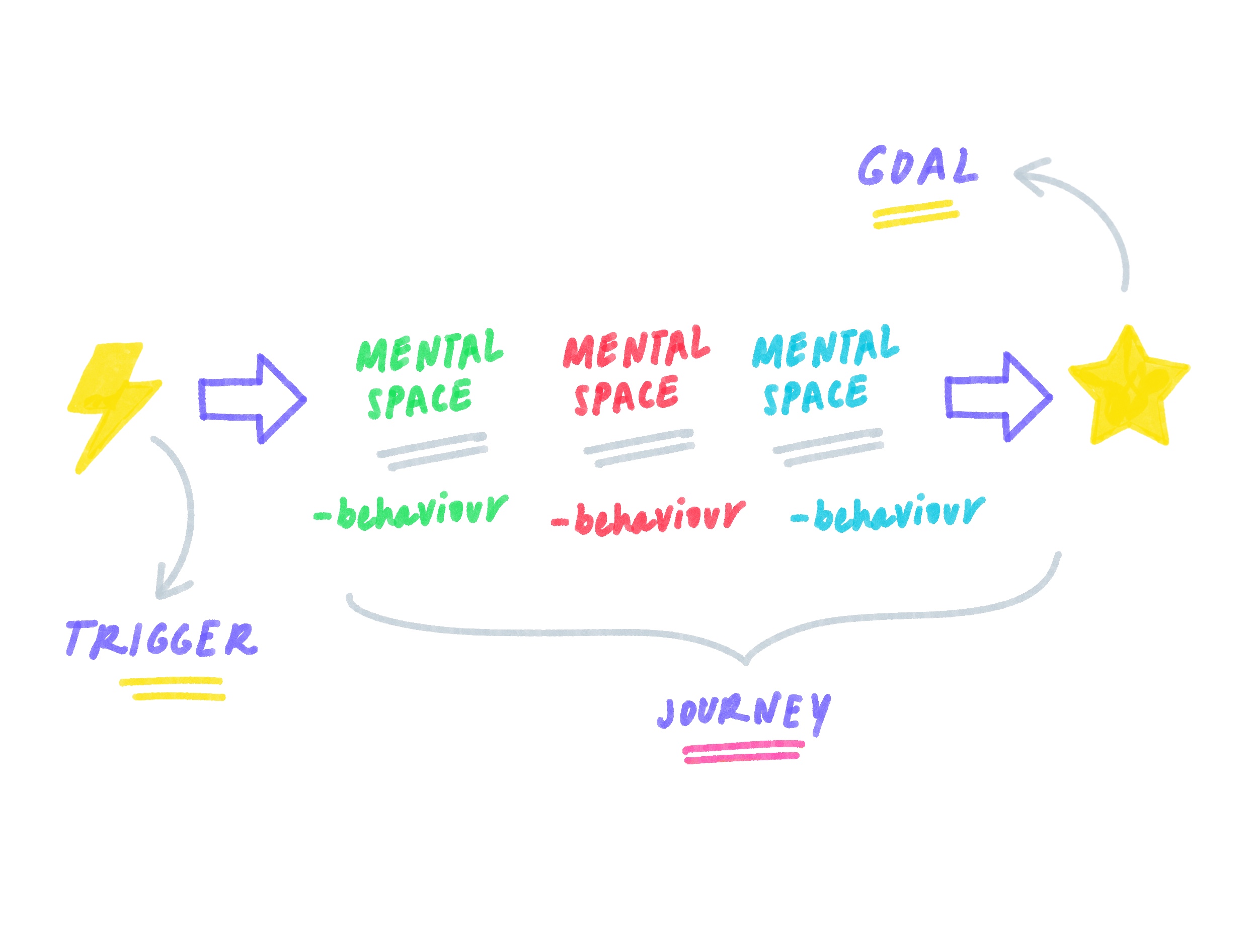
From patient care to the clinical experience, there are many aspects to designing digital products for healthcare. But in this post we’re going to focus on the patient experience - highlighting some of the tools already on the market and how they help improve the patient journey - from early intervention and consultations, diagnosis and treatment, through to on-going care and support.
Before we do that however, let’s first take a look at some of the design challenges faced by those designing for healthcare in general.

UX design challenges in healthcare
In no other field is the potential end user (in this case patients), nor the potential number of unique use cases quite so broad as it is in healthcare.
Age, location, gender, tech-savviness, language and level of education all impact design choices, and that’s before we even start to consider more general design accessibility for those with hearing, sight or other ailments that may impact the users’ ability. Inclusive design is therefore imperative in healthcare.
Fragmented use of technology and non-integrated services is one of the greatest challenges faced across the entire healthcare system with patients constantly having to explain the same issue to every doctor they see, or carry around a set of hand-written notes to each different appointment as is the case throughout pregnancy.
Furthermore, emerging technology (such as VR and wearable tech like heart rate monitors) present additional challenges as they can still be costly and not everyone has access. Utilising readily available technology that patients are likely to already have use of - although lowering the barriers to access - are, however, not without the challenges either.
Improving the interaction flow will always be key in healthcare (and beyond). Designing streamlined, simple interfaces are always a goal, but getting the right balance between ease-of use and meeting often stringent regulations can mean that we sometimes need to add a point of friction (for example, adding an extra ‘click’) so ensure there are no mistakes from the user.
But whereas this can help to ensure that the patient/clinician is reading the information they are provided with on screen, and aren’t just absent-mindedly clicking through from one step to the next, conversely, it could lead to users questioning “why spend so much money on a tool that makes it harder for users?” - especially when it might just seem quicker and easier to have a phone call.
A final issue that persists across all stages in the patient journey is security - or rather, ensuring data protection is maintained throughout their care. For example, whereas using apps and technology that patients naturally use in their day-to-day lives clearly has it’s benefits, they are unlikely to provide the requisite level of security that patients would want when it comes to details of their health getting into the ‘wrong hands’.
Digitising the patient experience
Ok, so now that we’ve covered some of the design challenges, let’s take a deeper dive into how digital tools (and good UX design!) can help tackle some key healthcare challenges whilst at the same time improving the patient experience.
We’ll also highlight some of our favourite examples for you to gain inspiration from as we go.

Prevention (& Early Intervention)
Truism as it may be, prevention really is better than cure. And this first stage in the customer journey is perhaps the area that offers most potential in terms of improving patient wellbeing - not least by helping prevent people from becoming ‘patients’ in the first place!
Lifestyle choices
Improving people’s lifestyle choices such as getting the right levels of physical activity and following healthy eating habits appears to be one of the most effective preventative measures. For example, did you know that 30-50% of cancers are preventable by healthy lifestyle choices?
It’s statistics like this that highlight the impact that improving people’s lifestyle choices could have - not just on individuals’ health and wellbeing, but also when it comes to the potential savings healthcare organisations (such as the NHS) could achieve if fewer people became ill in the first place as a result of poor lifestyle choices.
Though governments across the globe already provide information on topics such as healthy eating, quitting smoking, and getting daily recommended exercise, to support their populations in these areas, increased use of habit-forming apps - such as the NHS’ Weight Loss Plan, and Couch-to-5K - could help in this area.
Mental health support
Supporting people with mental health issues is another key area where early intervention is crucial to long-term health.
As recent data suggests that 1 in 4 people experience a mental health problem of some kind each year in England, it is perhaps no surprise that (in the UK at least) local NHS trusts, such as Oxfordshire, provide access to a wide range of health apps to support patients with mental health issues.
For example, Oxford VR currently provides virtual reality treatment/experiences for those suffering from fear of heights, and are soon to extend their offering to include programmes for depression and anxiety disorders including OCD and social anxiety.
We think this is a great initiative and example of where new technology can be used to good effect.
Consultations
The next stage in the patient journey is usually some form of consultation with a healthcare professional. Appointment booking is therefore another key stage in the patient journey that needs to be made as straightforward and stress-free as possible.
Appointment management
Missed GP appointments are costing the NHS millions every year in the UK. A stat which highlights just how much money can be saved through improving the system through which appoints are made, rescheduled and cancelled.
Thriva is a nice example of where apps can be used to ensure patients book - and attend! - regular check-ups with their GPs. Apps like Patient Access take this a step further, supporting a number of common actions like booking GP appointments and ordering repeat prescriptions.
Such tools are useful both in terms of improving the patient experience, and in reducing the administration burden on local health services.
Medical consultations
Beyond appointment booking, consultations are also being increasingly digitised. This is something the recent Coronavirus pandemic thrust into the limelight, with healthcare providers across the globe turning to remote consultancy methods - from phone calls, to virtual meetings, and even chatbots! - in response to lockdowns and stringent social distancing measures.
Even before this recent ‘need’ to adapt, the trend towards the use of “telemedicine” was fast growing. As we mentioned earlier, however, whereas some solutions - such as using WhatsApp to communicate with patients (as is common in Brazil) - may certainly increase accessibility, they aren’t without their pitfalls - data privacy and security in particular!
However, there are many examples out there of where it is being done right. Some of the best examples to draw inspiration from here include:
eConsult - who describe themselves as the “digital front door to healthcare, connecting everything to improve how we look after patients”, and is used by over 3,300 GP practices in the UK
Babylon - who use “AI and broader technologies” do deliver services through devices patients already own, and which doctors who use it report 3x higher job satisfaction than the wider clinical community
Nye - “Designed by clinicians, for clinicians”, this app makes clinician-patient communication simple, allowing calls to be made to any patient, on any device, from anywhere
On a more personal note, I’ve also had the opportunity to work on - and deliver a talk about - the Oxford Acute Referral System (OARS). This electronic system documents and manages the referral of patients to specialist services designed for the Oxford University Hospitals NHS Foundation Trust. (If you’re interested in learning more, you can watch the recording of the talk here.)
Diagnosis
Next up on our patient journey is diagnosis, and the importance of ensuring that the information given by medical practitioners is understood by the patients.
Health literacy
Alarmingly, recent data suggests that 61% of adults struggle to understand health information that includes both text and numbers. This highlights just how important it is that when communicating with patients, clinicians (and the broader healthcare and pharmaceutical industries) ensure that they present information, specifically on prescription medication, but also on healthy lifestyles and behaviours and educational brochures and leaflets in general.
Clear, reliable healthcare information is critical to ensuring that patients are able to make informed decisions about their care and support - in particular avoiding the use of jargon and unnecessary terminology that can prove confusing or intimidating to patients.
This is an area that we’ve worked on extensively for both Cognitant and Oxford University’s Nuffield Department of Primary Care Health Services.

Early detection of healthcare issues
Although lung cancer is the most common cause of cancer death, research shows that almost 9 in 10 will survive their disease for at least a year if diagnosed at the earliest stage.
It’s perhaps no surprise therefore, that we’re seeing the emergence of a raft of clinical artificial intelligence companies - such as Oxford-based Sensyne Health - that are working to tackle this particular issue.
Some of the most innovative solutions we’ve seen to date include early lung cancer decision support software, Optellum, autonomous echocardiography, Ultromics, and early asthma detection, Albus Health. It’s great to see healthcare professionals and software developers starting to combine their expertise in such ways.
Treatment
Once a diagnosis has been made, treatment is usually the next stage for the patient. However, it’s not uncommon for this to be another area of patient care where the experience can fall short of needs and expectations - and is certainly one that’s ripe for digital transformation.
For example, as the British Heart Foundation reports, of an estimated 28% of adults in the UK that have high blood pressure, more than half of them are not receiving effective treatment.
Treatment is an area where both the clinical and patient experience is being improved thanks to advances in technology. In the past decade, clinicians have gone from not having access to enough data, to having too much, resulting in less time being available to actually spend with patients.
Cancer care is an area that is particularly benefiting from next generation imaging software and decision support. For example, Mirada Medical has developed a range of tools that use AI and deep learning software which automates clinical processes.
By enabling faster, more consistent screening, this means radiotherapists and oncologists need to spend less time chasing and interpreting results, and have more time to spend with their patients - increasing their level of care and improving the overall experience.
Adherence to medication & new lifestyle
We move now to the final stage in the patient journey: adapting to new lifestyles and habits that support on-going recovery, health and wellbeing.
Again, this is an area of healthcare that has much room for improvement and is something that well-designed new technology can help support.
Take prescription medication as an example here. Surprisingly, it has been estimated that between 30% and 50% of medicines prescribed for long‑term conditions are not taken as intended. Reducing the number of relapses or need for additional treatment/operations is a surefire way to improve long-term healthcare as well as potentially saving £millions each year.
As with the healthy lifestyle apps we discussed earlier, finding ways to support patients adopt and adapt to new lifestyles is an area that has potential to make a big difference to so many people and with the right approach could be fairly simple to roll-out at scale with the right upfront investment and design.
MyGP and Echo Pharmacy are two such apps already available from the NHS. Healthera is another example that makes repeat prescription ordering simple and can be used to securely manage prescription ordering for the whole family.
What next for digital healthcare design?
It’s an exciting time to be working in UX design in healthcare right now. Few sectors have so much potential to not only design great user experiences, but also to potentially help save lives whilst doing so.
We’ve provided examples throughout this post to highlight some of the great ideas that are already being put into practice, but this barely touches the tip of the iceberg.
Of course, as we said at the outset, digital transformation is one thing, but without the right design, turning to digital apps could cause more problems than it solves - for patients and clinicians alike.
So, what’s next for digital healthcare design?
As we’ve seen, it’s clearly possible to create solutions that solve problem points at different stages of the patient journey. However, there are just too many potential journeys within each stage to design a service that works across the whole journey.
That leaves us with the big question of whether it’s possible to integrate these systems so that they make an even bigger difference to people’s health and patient journeys..?
A system that uses the best of emerging technology without excluding anyone.
A system that meets regulations and at the same time is innovative and easy to use - making the patient journey easier and better without introducing complexities that makes the flows so clunky and tiresome that people want to go back to/stick with manual systems.
A system that is efficient and saves precious time for our amazing healthcare services.
Whether that is something we’ll ever achieve is difficult to predict. But either way, we can’t wait to see what’s next!